Ask a Therapist In Tacoma: How to Get Better Sleep
Was sleeping better one of your New Year’s resolutions? If it’s already harder than expected, you’re not alone. Sleep struggles often have less to do with effort and more to do with how safe and predictable your nervous system feels.
In this post, a therapist in Tacoma breaks down realistic sleep hygiene tips that actually help—without turning bedtime into a performance. From morning sunlight and consistent wake times to calming self-talk, clock-watching traps, and Brainspotting therapy for deeper sleep blocks, this guide offers a compassionate, science-informed approach to better rest.
If you told yourself this was the year you’d finally get better sleep—go to bed earlier, stop scrolling, wake up feeling like a functional human—you’re not alone. And if that plan already feels a little derailed, you’re also very much not alone.
As a therapist in Tacoma, I work with a lot of thoughtful, capable people who are frustrated by sleep. They’re doing the right things, reading the articles, trying the tips—and still lying awake at night wondering why their brain won’t shut off. Most of the time, the problem isn’t effort. It’s that sleep is tied to your nervous system, your stress load, and how safe your body feels when everything finally gets quiet.
Let’s talk about sleep hygiene in a way that feels human, flexible, and actually doable—without turning bedtime into another self-improvement project.
Why Better Sleep Starts With Predictability (Not Perfection)
A lot of people assume better sleep means hitting the “right” number of hours every single night. In reality, your brain cares much more about rhythm than totals.
Consistent sleep and wake times help retrain your internal clock, even when some nights are short or restless. Trying to make up for lost sleep by sleeping in usually feels good in the moment—but it often makes the next night harder. Predictability builds safety, and safety is what sleep needs most.
Sleep Hygiene Tips That Calm Your Nervous System (Not Stress It Out)
1. Prioritize a Consistent Wake-Up Time
If sleep has been rocky, this is the single most important place to start.
Waking up at roughly the same time every day helps anchor your circadian rhythm and gives your body a reliable signal about when the day begins. Sleeping in after a rough night is understandable—but it can keep your sleep-wake cycle stuck.
Think of this as playing the long game. You’re teaching your body what to expect, not punishing it for a bad night.
Try to keep this consistent wake up time on the weekend too for best results.
2. Get Morning Sunlight (Yes, Even on Cloudy Days)
Morning light tells your brain, “This is daytime,” which helps melatonin arrive at night.
Clear/sunny days: Aim for 5–10 minutes outside
Cloudy days: Aim for 15–30 minutes
No sunglasses if it’s comfortable for your eyes
This could look like taking your dog for a morning walk, drinking your coffee on the porch, or standing near a bright window if going outside isn’t possible.
Stanford neuroscientist and podcaster Dr. Andrew Huberman has shared extensively on the benefits of morning sunlight for sleep and and general health and you can read more about his science-backed recommendations here.
3. Stop Clock-Watching When You Wake Up at Night
This one is deceptively important.
The moment you check the time, your brain tends to launch into calculations and predictions: “If I fall asleep right now, I’ll only get…” That mental math activates stress—and stress is the opposite of what sleep needs.
If you can, turn the clock away or keep your phone out of reach. Gently remind yourself that knowing the time won’t help you sleep—and not knowing might actually help.
4. Use Supportive Self-Talk When Insomnia Hits
What you say to yourself in the middle of the night can either settle your nervous system or wind it up further.
Instead of thoughts like “I’ll never fall asleep” or “Tomorrow is ruined,” try language that keeps things grounded:
“My body knows how to rest, even if sleep is lighter tonight.”
“I’ve handled tired days before.”
“This is uncomfortable, but I’ll be alright.”
These aren’t positive affirmations. They’re reminders that lower the sense of threat—which often helps sleep return on its own.
5. Don’t Try to Force Sleep
Sleep happens when your nervous system feels safe—not pressured.
The harder you try to make sleep happen, the more alert your body often becomes. If you’ve been awake for a while and feel tense or frustrated, it’s okay to get out of bed and do something low-key in dim light.
Experts recommend trying to fall back asleep for around 20 minutes if you wake up. If after that time you can’t fall back asleep, it can be helpful to get up. Staying in bed longer may reinforce sleeplessness. If you do get up, go into another room and do a boring activity like read a book, do breathing exercises or meditation, or try a puzzle like Sudoku until you feel drowsy.
Do not get on your phone, watch TV or engage with screens or bright lights, and don’t do an activity that is too stimulating. And don’t eat or drink anything except water. For more tips, check out this article from webmd.com.
The goal isn’t to distract yourself endlessly—it’s to remove pressure and let sleep come back naturally.
6. Create a Wind-Down Cue, Not a Perfect Routine
You don’t need an elaborate nighttime routine to sleep well.
One or two repeatable cues—lowering the lights, a cup of tea, stretching, a book, calming music, or a warm bath—can be enough to signal that the day is winding down. Simple habits that you actually stick with are far more effective than perfect routines you abandon after a week.
7. Watch Out for Sleep Tracker Obsession
Sleep trackers can be helpful—but they can also create anxiety.
"Orthosomnia is an unhealthy or excessive concern with achieving the perfect sleep," says Sabra M. Abbott, MD, PhD, a neurologist and sleep medicine expert at Northwestern Medicine who helped coin the term (How Tracking Your Sleep Can Make You Lose Sleep, NorthwesternMedicine.com)
If you notice yourself worrying about your sleep score, second-guessing how rested you feel, or feeling discouraged by the data on your watch, it may be doing more harm than good. Your body’s experience matters more than what an app reports.
Sometimes sleeping better starts with checking less.
8. Be Mindful of Caffeine Timing
Caffeine can linger in the system for 6–8 hours (or longer for some people).
If sleep is a struggle, experiment with cutting caffeine earlier in the day and notice—not judge—the difference.
Try a caffeine curfew of 2pm or earlier and adjust from there.
9. Regulate Stress During the Day
Nighttime is when unprocessed stress shows up.
Short daytime resets help:
Brief walks
Deep breathing
Stretching
Stepping away from screens
Calm doesn’t start at bedtime—it builds throughout the day. Check out this blog I wrote about nervous system regulating exercises you can try throughout your day.
10. Get Thoughts Out of Your Head Before Bed
A simple brain dump can reduce nighttime rumination. Multiple studies have shown that making a to-do list for your tasks tomorrow can promote faster and more restful sleep (Psychology Today).
Grab a journal and allow yourself to free-write, make a list, mind-map, doodle, or whatever you need to do to get your thoughts down on paper.
Write down anything that feels unfinished, stressful, or easy to forget. You’re not solving it—you’re giving your brain permission to rest by showing it the information is stored somewhere safe.
11. When Sleep Feels Stuck, Brainspotting Can Help
Sometimes sleep doesn’t improve even when habits are solid.
In those cases, the issue often isn’t sleep itself—it’s underlying nervous system activation. Brainspotting therapy works by helping the brain and body process stress, anxiety, or trauma that can keep you feeling wired at night.
As a therapist in Tacoma, I use Brainspotting with clients who experience racing thoughts, nighttime anxiety, or chronic insomnia. When the nervous system settles, sleep often becomes easier—without forcing or overthinking it.
If Sleep Is Still Hard, You’re Not Doing It Wrong
Better sleep isn’t about control—it’s about safety, predictability, and compassion.
Small, consistent shifts—paired with compassion and the right support—tend to go much further than rigid rules.
And if sleep continues to feel elusive, working with a therapist in Tacoma who understands sleep and nervous system regulation can help you rest without turning bedtime into another source of stress.
Ask a Therapist in Tacoma: How to set Goals that actually stick
Most New Year’s resolutions don’t fail because of laziness—they fail because they rely on motivation instead of systems. By February, even the most well-intentioned goals often fade, leaving people frustrated and self-critical.
Drawing from Atomic Habits by James Clear, this blog explores why small, 1% changes, realistic planning, and consistency matter more than grand resolutions. It also looks at what most goal-setting advice ignores: the nervous system, internal resistance, and the emotional blocks that can make change feel impossible.
From a therapist in Tacoma’s perspective, sustainable goals come from working with your brain and body—not against them. This post offers practical strategies and a compassionate approach to goal setting that actually lasts.
Why Your New Year’s Resolution Ghosted You
Tips from a therapist in Tacoma about setting goals that actually stick.
January is full of optimism. New planners. New gym memberships. New versions of ourselves who definitely wake up at 5 a.m. and love green smoothies.
And then… February hits.
The planner is abandoned. The gym bag is in your trunk judging you. And your New Year’s resolution quietly disappears without explanation.
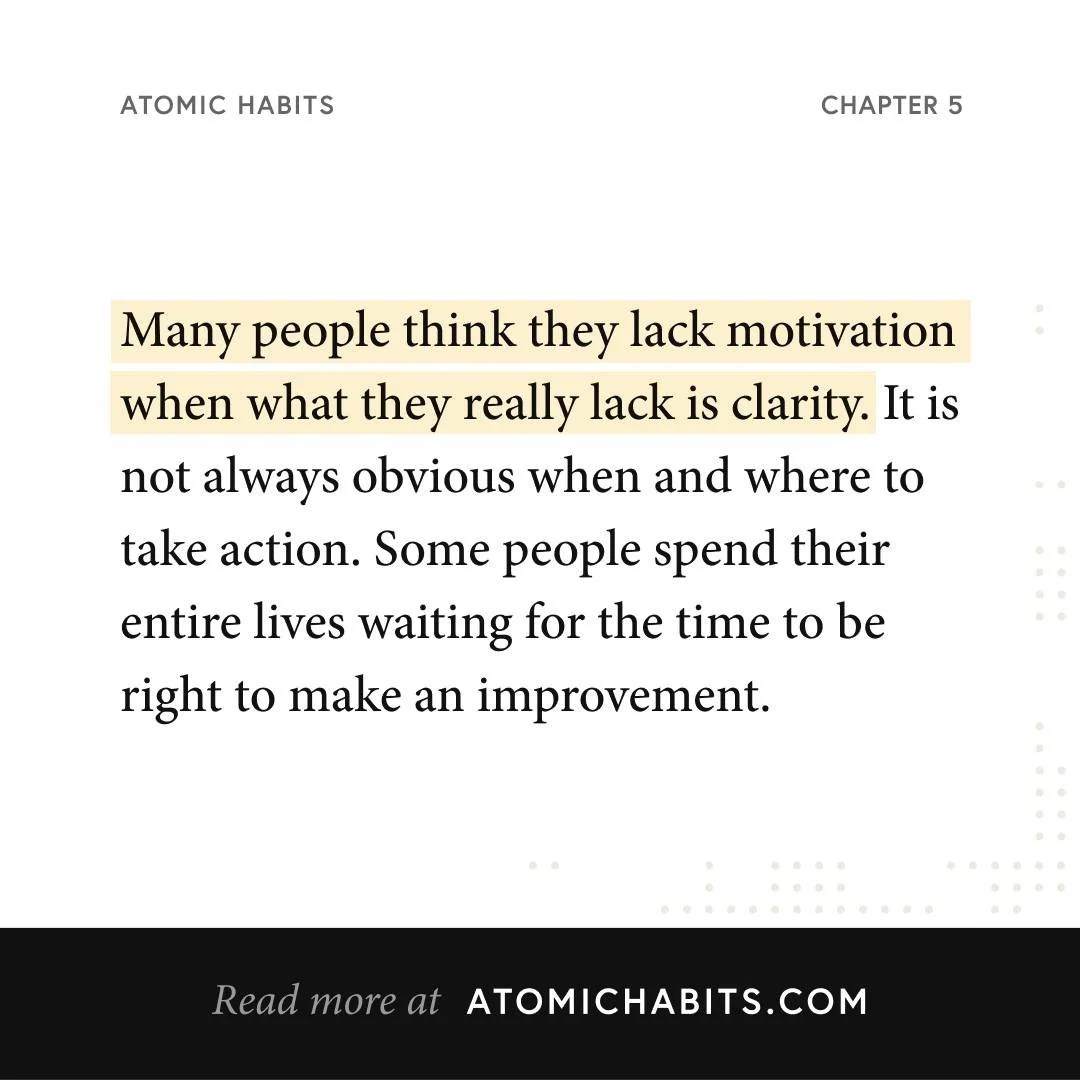
If this sounds familiar, you’re not lazy or broken. You’re just human—and probably setting goals the way most people do. As a therapist in Tacoma, I see this all the time. The problem usually isn’t motivation. It’s how the goal was designed in the first place.
Let’s talk about the difference between resolutions that fizzle out and goals that actually change your life—using best practices from one of my all-time favorite books, Atomic Habits by James Clear, plus a therapeutic lens (including Brainspotting therapy) to help you turn those January resolutions into lifelong lifestyles.
The Problem With New Year’s Resolutions
Most resolutions fail because they’re:
Too vague (“I want to be healthier”)
Too grand (“I’m going to completely reinvent myself”)
Too disconnected from daily life
Based on shame instead of values
They rely on willpower, which is a limited resource—especially if you’re already managing stress, trauma, anxiety, parenting, work, or all of the above.
A goal that only works when you feel motivated is not a sustainable goal.
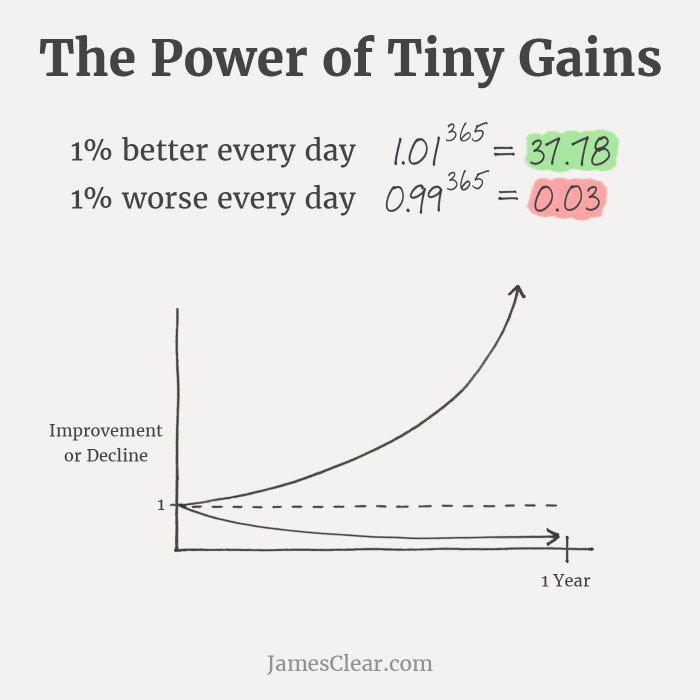
The 1% Rule: Small Changes, Big Identity Shifts
To read more about how tiny changes lead to huge life transformation, check out the book Atomic Habits by James Clear.
One of the most powerful ideas from Atomic Habits is this: getting 1% better every day compounds over time.
You don’t need to overhaul your life. You need to make the smallest possible change that you can repeat.
Instead of:
“I’m going to work out for an hour, five days a week”
Try:
“I’ll do 5 pushups every time I get up from my desk for a break.”
That might not sound impressive, but consistency beats intensity every time. Small habits don’t rely on hype—they rely on reality.
As a therapist in Tacoma, I can tell you this: the goals that stick are the ones that fit into your actual nervous system capacity.
Stop Setting Goals That Are Too Grand
Big goals aren’t bad—but skipping the middle steps is.
Your brain doesn’t resist change because it’s stubborn. It resists because massive goals feel unsafe, overwhelming, or impossible. When a goal feels threatening, your nervous system steps in with procrastination, avoidance, or self-sabotage.
Instead of focusing on the end result, ask:
What does the next smallest version of this goal look like?
What would “showing up imperfectly” look like?
For example, if you’re trying to write a book, let’s say ideally you’d love to write for an hour a day. The only problem is that you rarely have a full hour to devote to writing. And when you don’t, you tend to do nothing. “Oh well, I’ll write tomorrow.” THat’s a sure fire way to never finish your book.
Instead, lower the bar. Try this: “I’ll write one sentence every day.” Pretty soon, you’ve show up for one sentence but it easily turns into 100 words, then a page, then a chapter. Little consistent wins stack up.
Progress doesn’t come from pressure. It comes from approachability. Try lowering the bar—it’s not cheating, it’s effective goal setting.
Plan the Time and Place (This Is a big one!)
“I’ll do it sometime this week” is not a plan.
James Clear emphasizes that habits stick when you decide when and where they’ll happen. This removes decision fatigue and reduces the mental friction that leads to avoidance.
Try this formula:
“I will [habit] at [time] in [location].”
For example:
“I’ll journal for 3 minutes at 8:30 p.m. on the couch.”
“I’ll stretch for 5 minutes right after I shut down my laptop.”
Motivation is unreliable. Structure is not.
Habit Stacking: Let Your Existing Routines Do the Work
Connecting a new habit to an existing one is one of the most effective strategies for building a new routine.
Habit stacking means attaching a new habit to something you already do automatically.
Examples:
Before I drink my morning coffee, I drink one glass of water.
After I brush my teeth, I do 10 squats.
After I get into bed, I write one sentence in my journal.
You don’t need more discipline. You need better placement.
The “Never Miss Two Days in a Row” Rule
Perfection is the fastest way to quit.
Missing a day is normal. Missing two days is how habits quietly die.
This rule builds self-trust and flexibility at the same time. You don’t spiral into “I already failed, so what’s the point?” thinking. You just gently get back on track.
Consistency is not about never messing up. It’s a chance to learn from what went wrong, make changes, and picking it back up tomorrow.
When Goals Trigger Resistance: Where Brainspotting Comes In
Sometimes your resistance to a goal isn’t about time management—it’s about what the goal represents.
Therapy can help you identify areas of resistance, overcome obstacles, and hold you accountable to being your best self.
Common blocks I see as a therapist in Tacoma include:
Fear of failure or success
Old beliefs like “I don’t follow through”
Trauma stored in the body that makes change feel unsafe
Identity conflicts (“Who am I if I actually do this?”)
Brainspotting works directly with the nervous system to help process these deeper blocks. Instead of trying to “push through” resistance, Brainspotting allows your brain and body to resolve what’s underneath it.
Clients often notice:
Less avoidance
More clarity
A shift from self-criticism to self-trust
A felt sense of becoming the version of themselves they’re working toward
Goal setting isn’t just cognitive. It’s physiological.
From Resolution to Self-Actualization
The most sustainable goals aren’t about fixing yourself—they’re about becoming more of who you already are.
When you:
Make goals small enough to be doable
Attach them to your real life
Work with your nervous system instead of against it
Address internal blocks with tools like Brainspotting
…you stop relying on January motivation and start building identity-based change that lasts the long-haul.
your friendly neighborhood therapist in Tacoma is here to help.
If your resolutions haven’t worked in the past, that’s information—not a character flaw. With better systems, realistic expectations, and support for what’s happening beneath the surface, change becomes less exhausting and more natural.
If you’re curious about exploring goals, habits, or resistance patterns in therapy, working with a therapist in Tacoma who integrates Brainspotting can help you move forward in a way that actually feels sustainable.
Tips from a Therapist in Tacoma, WA: How to recover after doomscrolling
A therapist in Tacoma, WA shares 10 somatic and mental health exercises to help you reset after doomscrolling. Learn simple grounding tools to calm your nervous system, reduce anxiety, and reconnect with the present moment.
We’ve all been there: one minute you’re checking the news “for just a second,” and the next thing you know, you’re 40 minutes deep into doomscrolling, your shoulders are in your ears, and your brain feels like it’s sprinting a marathon it never signed up for.
If you’ve ever wondered why doomscrolling leaves you feeling anxious, depleted, or disconnected, here’s the quick explanation: your nervous system thinks the danger is happening to you right now. Even though you’re just staring at your phone, your body responds as if you’re on the front lines of every crisis you read about.
According to an article from Harvard Health:
“Doomscrolling is rooted in our brain's limbic system — often referred to as the lizard or reptilian brain — that's dominated by a structure called the amygdala. It promotes self-preservation and drives the fight-or-flight response to danger, fueling us to troll for threats.
"Stress stokes our primary urge to scroll," she says. "We're hypervigilant and scanning for danger. The more you scroll, the more you feel you need to."
When you catch yourself doomscrolling
We all know we need to cut back on our digital obsession. We need to put the phone down. We need to use apps like Freedom or devices like Brick to limit phone usage or time on socials. We need to be off devices first thing in the morning or before bed. But no matter how much good advice we get about disconnecting, we’re all guilty of succumbing to the dreaded doomscroll. And when that time comes, here are some tips about what to do about it.
I don’t think anyone has come up for air after a doomscrolling session and actually felt better about their life. If anything, snapping out of it feels like waking up from a really disorienting nightmare. Again, Harvard Health talks about the “popcorn brain effect":
“On a practical level, Dr. Nerurkar says, doomscrolling can give us "popcorn brain," which happens when we spend too much time online. "It's the real, biological phenomenon of feeling your brain is popping because you're being overstimulated online," she explains. "Then it's hard to engage with the real world, which moves at a much slower pace."
As a therapist in Tacoma, WA who works with clients navigating stress, overwhelm, and digital burnout, here are some practical grounding and somatic tools that can help reset the nervous system after a doomscrolling spiral.
Here are several simple, effective exercises you can do anytime you notice that you're stuck scrolling and feeling worse afterwards.
Set a “Re-Entry Ritual”
Choose one small thing you do every time you put down your phone after doomscrolling.
Examples:
Say out loud, “I’m back”
Stretch your arms overhead
Take a sip of water
Step outside for one deep breath
This signals to your brain that you’re shifting out of consumption mode and back into your real life.
Getting outside can be particularly powerful. A short walk around the block, or at least stepping outside for some fresh air can be a full-body reset that really helps change the channel in your brain after the numbing effects of doomscrolling.
Shake It Out (Literally)
Animals naturally shake after stress; humans tend to just store the tension.
Stand up and shake your hands, arms, legs, shoulders—whatever feels right—for at least 10–15 seconds.
This discharges excess adrenaline and softens that wired, buzzing feeling doomscrolling can create.
tapping and humming
Similarly, you can use your hands to pat or slap yourself comfortably all over your body. This tactile activation can feel soothing and help get you back in your body after a bout of doomscrolling. Notice what pressure feels good to you—light, or a little more forceful.
You can also pair it with humming. You can make a “voooooo” sound as you tap around your torso, or on your arms, etc. The vibration of the humming is stimulating for your vagus nerve, which runs from your brain down to your belly.
Squeezing or brushing the body
Another technique involves using your hands to gently squeeze different parts of your body briefly. Giving a quick squeeze to your arms, along your legs, to parts of your torso, glutes, etc. is another way of releasing energy and getting more present in your body.
In addition, you can use your hands to brush across your skin in a similar method. As if you’re brushing leaves off your clothes or something, do this all across your limbs and trunk.
Notice as you tap, hum, squeeze, and brush how these different movements feel to your body. The gentle pressure should feel grounding and pleasant. You can also have a partner do these actions to you as well.
arm swings with exhales
After doing the tapping, squeezing, and brushing exercises, you can try simultaneously raising your arms above your head, and swinging them down together in unison by your sides, while breathing out a forceful exhale. Inhale as you bring your arms up again, and then exhale as you swing them down quickly to your sides. Repeat this 8-10 times.
See these somatic exercises in action
To see all of these practices strung together, check out this video from Johns Hopkins Medicine about how to use these somatic exercises to get your brain out of the functional-freeze-state of doomscrolling and get your body more regulated. The exercises start at minute 3:57 in the video.
This video from Johns Hopkins Medicine shows a few somatic exercises grouped together than can help you regulate your nervous system after doomscrolling
Here’s a list of more somatic exercises that with emotional regulation that you can try from Johns Hopkins Medicine:
https://www.hopkinsmedicine.org/office-of-well-being/connection-support/somatic-self-care#shorts
The 5-4-3-2-1 grounding Reset
A quick grounding technique that brings you back to the present moment.
5 things you can see
4 things you can touch
3 things you can hear
2 things you can smell
1 thing you can taste
This moves your attention out of digital stress and into your real environment.
Taste and smell can be particularly powerful ways to get us back into our bodies, so don’t skip over those. (I have clients that swear by tasting something super sour like a Warhead to instantly get them out of a spiral and into a more grounded state—try it!)
Box Breathing
Inhale for 4, hold for 4, exhale for 4, hold for 4.
Repeat 4–6 times.
This is one of the fastest ways to flip your brain out of fight-or-flight and into regulation.
The “Phone Down, Feet Down” Technique
Put your phone on a table or counter—somewhere not in your hand.
Then plant both feet firmly on the ground.
Feel the weight of your body, the floor supporting you, and your breath.
This simple act creates a physical boundary between you and the digital spiral.
Quick Body Scan
Starting at your forehead and moving downward, ask:
“Is there tension here?”
“Can I soften it by 5%?”
Micro-relaxation works even if you can’t fully let go of tension. Repeat this process til you feel a shift.
Cold Temperature Reset
A splash of cool water on your face or placing something cold on the back of your neck activates the mammalian dive reflex.
This naturally lowers your heart rate and calms stress signals.
Similarly, you could take a cold shower, or even just step outside into the cold air for a quick reset.
The 2-Minute Refocus List
Grab a sticky note or your Notes app (but don’t scroll!).
Write:
One thing you can control
One thing you’re grateful for
One small task you can do next
This breaks the helplessness that doomscrolling often fuels.
five-minute timer activity change
It can be hard to shift gears into action after doomscrolling, so overcome the inertia of moving again by setting a five-minute timer to start doing something physical. It could be washing the dishes, a productive task, taking a walk outside, even doing some light stretching, or moving to music. Start with 5 minutes, and you may find when the timer goes off you feel capable of doing more and continuing to switch up that energy.
If Doomscrolling Is Affecting Your Mental Health, You’re Not Alone. therapy in tacoma, wa can help.
Therapy in Tacoma, WA and WA state to help with anxiety and emotional regulation.
Modern stressors hit differently when you carry them in your pocket. If you notice that your mood, sleep, or attention is getting pulled into nonstop digital overwhelm, mental health therapy can help.
Working with a therapist in Tacoma, WA can give you personalized tools to regulate your nervous system, set healthier phone boundaries, and navigate the emotional impact of constant online news.
If you're ready to feel more grounded, more present, and more in control of your mental health, therapy is a great place to start. Brainspotting in particular is a somatic therapy that can get to the root of dissociative behaviors like doomscrolling and help you make the changes to your mood and behavior that you want to experience long-term. Click below to learn more about how brainspotting therapy in Tacoma, WA could help you.
Finding Hope After Trauma: One Man’s Journey with Brainspotting Therapy
Sometimes, talk therapy isn’t enough. Especially when we are trying to heal from trauma. For many people living with PTSD, it is too painful to have to recount the details of their painful experiences. If you’re looking for a therapist in Tacoma, WA to help you heal from trauma, I can help. Brainspotting therapy is an alternative to talk therapy that can be more effective. Brainspotting works with the part of the brain that stores traumatic memories and regulates our nervous system. It uses a method to help people heal without having to relive all of the painful details. Read the blog to watch the video testimony of one client’s healing experience with brainspotting therapy.
For many people, trauma isn’t something that stays in the past. It can show up in daily life — through flashbacks, anxiety, nightmares, or even the constant feeling that you’re never truly safe. Many people suffer the negative impact of PTSD affecting their daily life for years, even decades.
what to try when talk therapy didn’t work for you
Many people seek out a therapist in Tacoma, WA to help them heal from PTSD and find relief. For some, they find what they are looking for right away. But for others, they may find that therapy is not as effective as they were hoping for. This can be for many reasons. Maybe the therapist wasn’t the right fit. Or maybe the therapy itself wasn’t what they needed.
This can sometimes be people’s experience with talk therapy. If you’ve ever felt like going to therapy is just talking about the problem without ever really solving it or changing anything, then this blog is for you.
one client’s experience with brainspotting therapy
Fortunately, there is hope for healing from trauma. Cutting-edge therapies like EMDR, brainspotting, and other somatic therapies can dramatically reduce the symptoms of trauma and make healing possible. And it doesn’t have to take years.
Today, I want to share the story of one man’s experience with brainspotting and how it changed his life. This is not one of my clients. I came across this man’s testimony in a brainspotting training. But I wanted to share it with you in hopes that it can inspire you in your own healing journey and help you understand how brainspotting therapy in Tacoma, WA may be able to help you.
After surviving severe childhood trauma, Ted spent years battling the symptoms of post-traumatic stress disorder (PTSD). His journey included inpatient psychiatric care, ongoing therapy attempts, and even moments of wrestling with suicidal thoughts. While he desperately wanted healing, traditional approaches to therapy never seemed to create the relief he hoped for.
When Talk Therapy Feels Too Painful
Like many trauma survivors, he tried several rounds of therapy over the years. Some of these approaches were talk therapy or cognitive processing therapy — methods that asked him to share or analyze the painful details of his abuse. But for him, talking about the past wasn’t just difficult; it felt nearly impossible.
The thought of revisiting those dark memories left him feeling stuck and overwhelmed. Therapy sessions sometimes felt more retraumatizing than healing, and he began to believe that maybe nothing could really help.
This is a common experience for trauma survivors. Wanting relief but feeling unable to talk through the details can leave someone feeling like their healing is out of reach.
Discovering a Different Kind of Therapy—brainspotting
Everything shifted when he heard about brainspotting therapy. What appealed to him about this was that he didn’t have to rehash every detail. He could engage with the healing process without having to talk it to death, again.
Brainspotting is a therapy that works with the body and the brain’s natural healing processes. Instead of relying only on words, it helps access where trauma is stored in the nervous system, working with both the mind and the body. For people who feel blocked or overwhelmed by talking, brainspotting offers a gentle but effective alternative.
In the video, Ted shared that this was the first time he felt truly hopeful about therapy. Knowing he could engage in the process without being forced to relive the details of his abuse gave him the courage to try again.
A Breakthrough After Years of Struggle
The results came quickly. After just three sessions of brainspotting therapy, he noticed a dramatic reduction in his PTSD symptoms.
The nightmares, the constant hypervigilance, the heavy sense of being trapped in the past — all of these began to lift. For the first time in decades, he felt like himself again.
His relief was so profound that he now wants to share his story with others. After years of believing he was beyond help, he discovered that healing was possible in a way he never expected.
Not everyone will experience healing this quickly or as dramatically. Each person is different. But because of how brainspotting works with the brain and nervous system, it can help many clients get results that were never possible for them with talk therapy alone.
Why Brainspotting Works Differently
Brainspotting therapy is not magic, but it works differently than many traditional talk therapies. Instead of requiring you to explain every detail of what happened, brainspotting uses the connection between the eyes, brain, and body to find “brainspots” — places where traumatic experiences are stored.
When guided in a safe and supportive environment, the brain naturally begins to process and release what has been held for so long. This allows healing to happen without needing to go into the full narrative of your trauma if that feels unsafe.
For trauma survivors who feel like words fail them, this can be a game-changer.
Therapy in Tacoma, WA That Meets You Where You Are
Ted’s story is unique, but it reflects what many people in Tacoma, WA experience when they’re searching for therapy. Some feel like they’ve “tried everything,” only to be left frustrated and discouraged. Others worry that they’ll have to tell every detail of their story just to begin healing.
But therapy doesn’t have to be that way. Brainspotting provides another path forward — one that respects your readiness, your pace, and your need for safety.
An Invitation to Take the Next Step and find a therapist in Tacaoma, wa
If you’ve been living with the weight of trauma, you may know how isolating it can feel. But you are not alone — and there are therapies like brainspotting that can truly help.
If this story resonates with you, I invite you to learn more about how brainspotting therapy in Tacoma, WA can support your healing. You don’t have to relive every painful detail in order to move forward.
When you’re ready, I welcome you to explore my specialty page on brainspotting therapy to see how this approach might be a good fit for you. Healing is possible — and you don’t have to do it alone.
Ask a Tacoma Therapist: What if “Talk therapy didn’t work for me?” and why brainspotting therapy might
If talk therapy hasn’t helped you feel better, you’re not alone. But don't write off therapy yet. You probably just need a body-based approach. Brainspotting therapy in Tacoma, WA offers a gentle, somatic approach to healing trauma, grief, and anxiety—especially when emotions feel stuck in your body, not just your mind. Learn how this powerful therapy can help you move forward.
I’m Kate Hagborg, LMHC with Destiny City Counseling, and I offer in-person therapy in Tacoma, WA and online therapy in WA state.
what if talk therapy didn’t work for me?
If you’ve tried traditional talk therapy and left feeling frustrated, disconnected, or like nothing really changed—you’re not alone. Many people find that while talk therapy offers insights, it doesn’t always lead to the deep healing they need. This is especially true for trauma, grief, or anxiety that seems to live in your body just as much as in your thoughts. If you’ve ever said, "I understand why I feel this way, but I still feel stuck," brainspotting therapy may be what you’re looking for.
Brainspotting therapy is different than talk therapy
Brainspotting is a somatic, body-based approach to therapy that focuses on where in your body you feel your emotional pain. It doesn’t rely solely on words or logical understanding. Instead, it gently invites your nervous system to process and release stuck trauma at the subcortical level—the part of the brain that controls emotion, memory, and instinct.
Unlike traditional talk therapy, which often stays in the rational part of the brain, brainspotting helps clients access deeper, pre-verbal experiences stored in the body. It respects your pace and doesn't require you to talk through every detail of your trauma. Instead, it meets you where your pain actually lives—in your chest, your gut, your jaw, your nervous system.
Why this matters—trauma lives in the body
Talk therapy can sometimes feel like you’re saying all the right things but not actually feeling better. That’s because trauma doesn’t just live in your memories—it lives in your body. You may experience tightness in your chest, a pit in your stomach, or a sudden wave of anxiety and not understand why. Or maybe you feel, numb, disconnected, or unable to stop addictive behaviors like doom-scrolling or emotional eating. These are signs your nervous system is holding onto something that talking alone can’t reach.
Brainspotting offers a way to bring compassion and attention to those physical sensations. It helps the body complete stress responses that were interrupted during traumatic or overwhelming experiences. In my work as a therapist in Tacoma, WA, I use brainspotting to help clients gently access these deeper layers, especially when other approaches haven’t helped.
how brainspotting therapy helped Kathleen Ferraro process her grief
Self Magazine recently published an article (June 4, 2025) titled ‘Brainspotting’ Was Life-Changing for Me. Here’s What to Know About the New-ish Therapy Technique by Kathleen Ferraro. In it, she describes her personal experience:
In the June 4, 2025 article for SELF Magazine titled ‘Brainspotting’ Was Life-Changing for Me. Here’s What to Know About the New-ish Therapy Technique, Kathleen Ferraro describes how brainspotting therapy changed her life.
“After my dad died unexpectedly, nothing seemed to touch the emotional and physical weight of the grief. It lived in my body—tight in my chest, heavy in my stomach, painful in my muscles. Traditional therapy felt like talking in circles. Grief counseling fell flat. But brainspotting? That cracked something open.
Kathleen's words are something I hear often in my Tacoma counseling office: that people feel like they’re walking around with unresolved emotional weight and don’t know how to unload it. Brainspotting therapy allows us to access that grief in a way that honors both the mind and the body.
how does brainspotting therapy work?
In a brainspotting session, I help clients find a "brainspot"—a specific eye position that corresponds to where trauma or emotional pain is held in the body. This spot is often identified by noticing physical sensations that arise while discussing a painful experience. Once we locate the brainspot, you simply observe your internal experience as your body and nervous system process it.
As Kathleen Ferraro described:
“In my first session, my therapist asked me to focus on a specific point on the screen—a seemingly random spot she’d identified after I described the sickening sensations I felt while talking about a recurring nightmare tied to losing a parent. I stared, and suddenly, I felt it: My stomach twisted, my body tensed, and a wave of panic washed over me. It was like the grief had been frozen in my nervous system, and now it finally had room to move.”
There is no need to relive every detail of a traumatic memory. Instead, the focus is on allowing physical and emotional sensations to emerge, be noticed, and move through the body. Ferraro writes:
“As you focus on the brainspot, physical sensations tied to your trauma begin to surface,” says Dr. Kaylor. For me, that often meant a racing heart, tight muscles, nausea, and difficulty swallowing. My therapist would then prompt me to notice, name, feel, and sit with these sensations without trying to push them away.
Brainspotting is believed to access the brain’s subcortical areas—those responsible for instinct, memory, and emotion—which allows stuck trauma to be released in a way that feels organic and compassionate
What results should I expect from brainspotting?
Brainspotting therapy can help the body release stored trauma and help regulate the nervous system.
Everyone’s experience with brainspotting therapy is unique. Some people feel a shift after just a few sessions. Others with more chronic trauma, dissociation, or long-standing patterns may notice more subtle changes that build over time. Sessions can be done in-person or online and still be highly effective.
Clients I work with often describe a softening of their inner world—less reactivity, fewer panic attacks, more connection to their emotions, and a deeper sense of calm. One client told me, "It’s like I have access to parts of myself I didn’t know how to reach before."
Kathleen Ferraro echoes this in her article:
“Though it took longer for me to reap the benefits of brainspotting, it was worth the wait. After four months of weekly brainspotting sessions, my flashbacks and nightmares noticeably decreased—what used to happen every week now occurred only every few months. The intense waves of grief also softened. Instead of stopping me in my tracks, the feelings became something I could sit with and move through, allowing me to return to my day without being swept into a full-blown panic response.”
how to know if I’m a good fit for brainspotting?
Brainspotting therapy might be right for you if:
Talk therapy hasn’t worked or felt like enough
You struggle to articulate or even understand what you’re feeling
You want relief from trauma without having to retell the whole story
EMDR didn’t feel like a good fit for you
You feel like your body is holding onto stress, anxiety, or pain
You want to become more compassionate toward yourself
Whether you're dealing with grief, anxiety, trauma, or just feel stuck, brainspotting therapy offers a gentle but powerful path forward.
Kate Hagborg, LMHC is a certified brainspotting therapist in Tacoma, WA
about the author
Kate Hagborg, LMHC is a certified brainspotting therapist in Tacoma, WA. She offers sessions in-person therapy sessions in Tacoma, WA, or virtual therapy sessions in WA state.
I integrate brainspotting and somatic work with a trauma-informed, relational, and spiritually-sensitive lens. You can learn more about my approach here. My other specialities include anxiety, burnout, codependency, and people-pleasing.
If you're curious about brainspotting therapy in Tacoma, WA, I invite you to reach out for a free 15-minute consultation. I’d love to talk with you about whether this approach might be a good fit for your healing journey.
To read more about brainspotting therapy, check out these other articles:
Ask a Therapist in Tacoma, WA: How to Regulate Your Nervous System
Feeling anxious, overwhelmed, or emotionally stuck? Your nervous system may be the key. In this in-depth guide from a therapist in Tacoma, WA, we explore how nervous system regulation supports emotional balance, resilience, and healing. You’ll learn how chronic stress and trauma impact the body, why common reactions like anxiety or shutdown are rooted in survival, and how brainspotting therapy can help rewire old patterns from the inside out. Whether you're looking for practical tools like breathing techniques and grounding exercises, or how to build your window of tolerance, this post offers compassionate insights and actionable steps. Discover how therapy provides a safe relationship where your nervous system can begin to feel calm and connected again.
Find a therapist in Tacoma, WA today and learn tools to start regulating your nervous system.
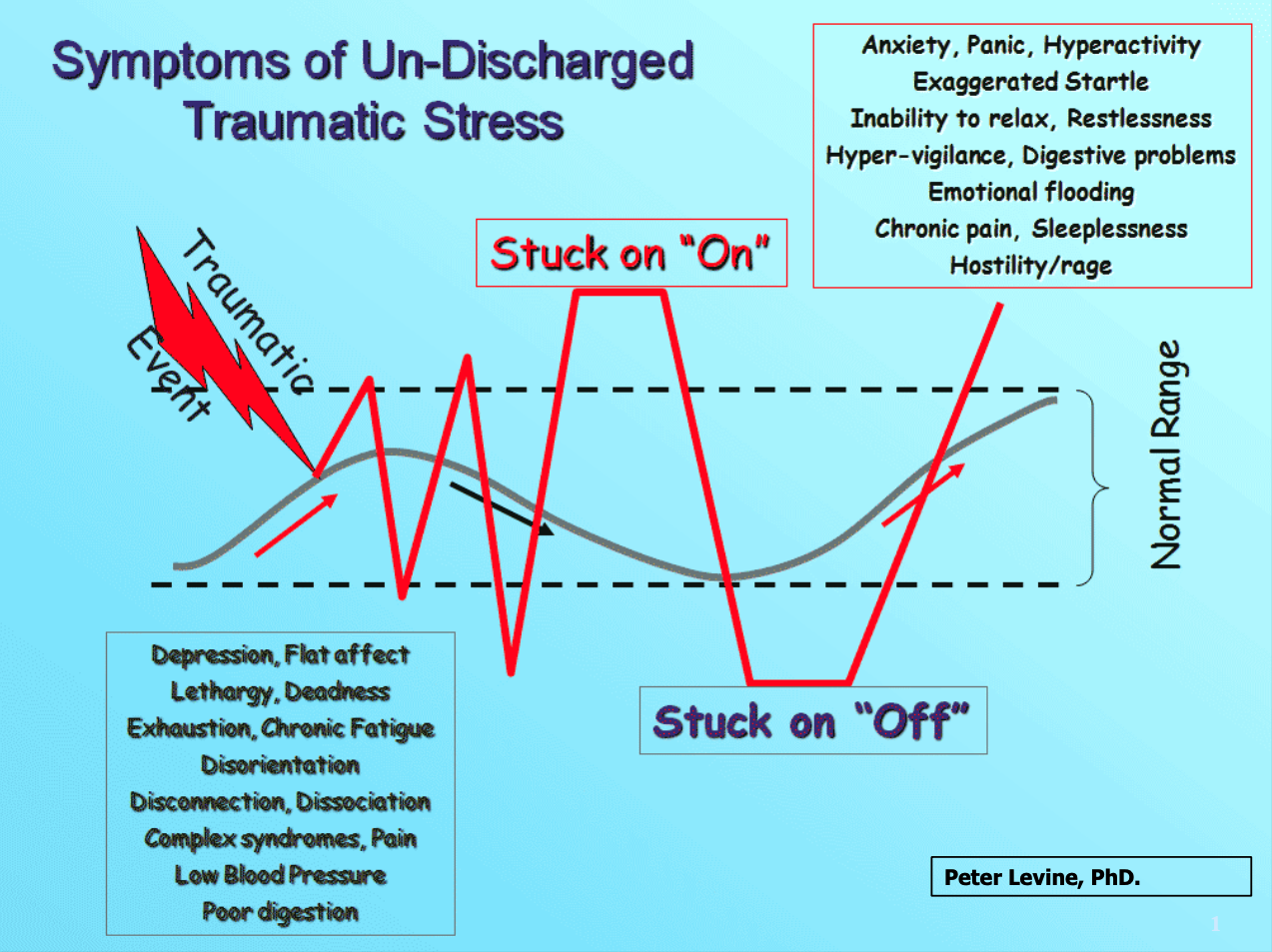
If you’ve ever felt anxious, on edge, or exhausted for no clear reason, your nervous system may be trying to tell you something. In my work as a therapist in Tacoma, WA, I often help clients understand how their emotional and physical responses are connected to their nervous system—and more importantly, how to support regulation. Whether you’re recovering from stress, trauma, or just trying to find more balance in daily life, learning to regulate your nervous system is foundational to feeling safe, calm, and connected. In this post, we’ll explore what nervous system regulation is, why it matters, and how therapy—especially brainspotting therapy—can help you feel more grounded and resilient.
What Does It Mean to Regulate Your Nervous System?
Regulating your nervous system means being able to return to a calm, centered state after experiencing stress. It’s not about avoiding stress altogether, but rather being able to move through it without getting stuck in fight, flight, freeze, or fawn responses. A regulated nervous system allows you to feel emotions without being overwhelmed by them.
Imagine you're at work and receive an upsetting email. If you're dysregulated, you might lash out, shut down, or obsess about it for hours. If your system is regulated, you can notice your reaction, breathe through it, and respond thoughtfully. Therapy helps you build this capacity.
Why Nervous System Dysregulation Happens
Dysregulation can occur when your nervous system gets stuck in survival mode due to chronic stress, trauma, or lack of safety in your environment. Over time, this can lead to patterns of anxiety, irritability, shutdown, or feeling numb.
For example, growing up in a chaotic or critical household can prime your nervous system to stay on high alert. Even long after the threat is gone, your body may react as if it’s still there. Working with a therapist in Tacoma, WA can help identify and interrupt these patterns, creating space for healing and new responses.
The Role of the Autonomic Nervous System: Fight, Flight, Freeze, and Fawn
The autonomic nervous system has two main branches: the sympathetic (activating) and parasympathetic (calming). When danger is perceived, your system may respond with fight or flight (sympathetic), or freeze and fawn (parasympathetic in a shutdown mode).
For instance, fight might look like anger, while fawn might mean people-pleasing to stay safe. Therapy can help you better understand these responses and work with them, not against them.
What’s cool is that the brain has a “switch” (metaphorically speaking), to toggle between its active and calming state. It can only be in EITHER sympathetic or parasympathetic—which means that focusing on calming coping strategies can force the switch to flip and enable us to soothe our nervous systems faster. These strategies are not instantaneous, but stick with them and they will make a noticeable impact.
Signs Your Nervous System Might Be Dysregulated
Some signs include chronic anxiety, trouble sleeping, difficulty concentrating, feeling emotionally numb, or sudden mood swings. You might also notice physical symptoms like headaches, digestive issues, or chronic tension.
If this sounds familiar, you’re not alone—and there’s support available. A therapist trained in nervous system regulation and brainspotting therapy can help you connect the dots and start feeling better.
You can check out this previous article for more information on how to recognize a dysregulated nervous system.
How Therapy Helps Support Nervous System Regulation
One reason therapy is so powerful is because of co-regulation. The nonanxious, supportive presence of another person helps to regulate our nervous system so we can heal faster.
Therapy provides a safe, structured environment where you can explore your triggers and responses with curiosity rather than judgment. It also offers a consistent relationship where your nervous system can begin to feel safe.
Through guided exploration, you can develop body awareness, track your responses, and gently reprocess old wounds. Modalities like brainspotting therapy allow us to target the body-based aspects of dysregulation and help you return to balance.
Brainspotting and Nervous System Healing
Brainspotting therapy is a powerful tool that accesses deeper parts of the brain tied to trauma and emotional memory. By identifying a "brainspot"—a specific eye position linked to unresolved experiences—we can facilitate healing at the nervous system level.
One client described it as "getting to the root of the feeling without having to talk it to death." Many clients find that brainspotting allows for release without needing to relive the trauma. In sessions, we create a calm container where your body leads the process.
Small Changes, Big Impact: The Power of Daily Regulation Practices
You don’t have to overhaul your life to start feeling better. Gentle, consistent practices like stretching, walking in nature, or mindful breathing can support your nervous system’s resilience.
Even five minutes a day of slow breathing or quiet reflection can begin to shift your baseline. These tools become even more effective when introduced and supported in therapy, where we personalize them for your needs.
Breathing Techniques That Actually Work
Breathwork is a helpful way to switch from panic-brain to calming-brain. Therapy can help you learn tools like this to regulate your nervous system.
Simple breathing exercises, like box breathing (inhale 4, hold 4, exhale 4, hold 4) or extended exhales (inhale 4, exhale 6-8), signal to your nervous system that you are safe. These tools may seem small, but they’re powerful.
In therapy, we often practice these together so you can feel the difference in real time. A therapist in Tacoma, WA can help you find the version that feels most natural to you.
Here are some free breathwork videos that you can try on your own:
Grounding Exercises for Moments of Overwhelm
Grounding techniques help bring your body back to the present moment. Try naming five things you see, four you can touch, three you hear, two you smell, and one you taste.
This sensory awareness interrupts spirals of anxiety or dissociation. Practicing these with a therapist makes it easier to use them when you need them most—and to trust that they work.
Here’s a free video that walks you through the 5-4-3-2-1 Grounding Technique.
Movement and the Mind-Body Connection
Movement helps release stress stored in the body. Gentle stretching, yoga, walking, or even dancing can signal to your nervous system that it's safe to let go.
Nutrition, Sleep, and the Nervous System
Daily habits like hydrating, meal prep, and showering can be hard when we are depressed. Therapy can help you find a routine to start feeling better faster.
Food and rest have a direct impact on how your nervous system functions. Blood sugar crashes or poor sleep can make emotional regulation harder. Too much caffeine can exacerbate anxiety, panic attacks, and sleep issues.
And how many of us are guilty of not drinking enough water? This one’s always a struggle for me. But dehydration can lead to brain fog, tiredness, fatigue, headaches, and more. Water is necessary for our cells and bodies to do just about every process they are designed for.
Depression and anxiety can make it difficult to develop daily routines. You may struggle with activities of daily life like getting adequate nutrition, over-eating or binge eating, not having the bandwidth to hydrate, grocery shop, or stay consistent with these things. This is nothing to be ashamed of—it’s just a sign your nervous system is overwhelmed and you could use some more support.
Therapy often includes conversations about lifestyle patterns that support your mental and physical health. We might explore how caffeine, screen time, or meal timing affect your sense of balance. We can help you develop a plan to address your physical needs that isn’t overwhelming and starts to help you feel better.
Why You Can’t “Think” Your Way Out of Anxiety
Cognitive tools like reframing or positive self-talk are useful—but they aren’t always enough. That’s because anxiety often lives deeper in the body than in the rational mind. When your nervous system is activated, the logical parts of your brain may go offline.
For example, you may know intellectually that you're safe, but your heart is racing, your muscles are tense, and your thoughts are spiraling. In these moments, telling yourself to "just calm down" often doesn’t work.
In therapy, especially using brainspotting, we bypass the overthinking and work directly with the body's response. We allow your system to express and resolve the anxiety at its root—physically and emotionally.
Co-Regulation: Why We Heal Better with Others
Regulation isn’t just a solo task. Our nervous systems co-regulate through safe relationships. This is why therapy can be so healing—because it provides an ongoing opportunity to experience safety and attunement.
Think about how a baby calms when held by a caregiver. Adults aren’t so different. Sitting with someone who is grounded and empathetic can help your system calm down. That’s part of what I offer as a therapist in Tacoma, WA—a stable, attuned presence that supports your healing.
Building a “Window of Tolerance” for Stress
Your window of tolerance is the zone where you can think, feel, and function without becoming overwhelmed or shutting down. Outside of this window, you might feel frantic, angry, or shut down and frozen.
In therapy, we help expand that window over time. We practice staying present with emotions that used to feel intolerable. Through techniques like brainspotting, resourcing, and titration, we slowly build your capacity to stay grounded during stress.
Self-Compassion as a Regulation Tool
Self-compassion isn’t just nice—it’s a powerful regulator. Harsh self-criticism increases cortisol and adrenaline. Kindness and acceptance, on the other hand, soothe your nervous system and promote healing.
One client I worked with started writing daily compassionate notes to herself. Over time, she noticed her anxiety lessened—not because her life got easier, but because her inner world became a more supportive place.
If being kind to yourself feels foreign, therapy can help you build that muscle.
How to Talk to Kids About Their Nervous Systems
Therapy is the gift that keeps giving generation after generation! Learning how to regulate your nervous system is one of the best parenting practices that can help your kids.
Our relationship to our nervous system doesn’t just affect us. Learning how to regulate better makes us more present and attuned parents, caregivers, and teachers. Teaching kids about their nervous systems helps them build emotional resilience. Using simple metaphors—like calling the brain a "guard dog" or describing nervous system states as "zones" (red for angry, blue for sad)—can help them understand what’s happening inside.
For example, a parent might say, "It seems like your engine is running really fast. Let’s take some slow breaths to cool it down." These conversations help kids feel empowered rather than ashamed. Getting support for yourself first is the number one things you can do to help set your kids up for success when it comes to mental health. You can translate what you learn into tools that are age-appropriate and effective for the little ones in your life.
Nervous System Regulation in Trauma Recovery
Trauma disrupts the nervous system’s ability to feel safe. That’s why trauma recovery isn’t just about talking—it’s about helping the body feel safety again. Brainspotting therapy is especially helpful for this because it allows the body, not just the mind, to lead.
One trauma survivor I worked with described feeling like her body "finally exhaled" after a lifetime of tension. Therapy gave her a space where she didn’t have to explain everything—she could just feel and heal.
Recovery is possible, and it begins with helping your nervous system rediscover safety.
When to Seek Help from a Therapist in Tacoma, WA
If you find yourself feeling stuck, exhausted, overwhelmed, or emotionally numb more often than not, it may be time to reach out. Or if all your energy is spent supporting others in your life, but there’s not enough left in the take to care for yourself well, therapy can help you. You don’t need to be in crisis to benefit from therapy—supporting your nervous system can be a proactive form of self-care.
A therapist in Tacoma, WA can help you make sense of your symptoms, identify helpful tools, and build a personalized path toward regulation and healing. It’s okay to ask for help—it’s actually a sign of strength.
Final Thoughts: You’re Not Broken—Your Nervous System Just Needs Support
So many people walk through life feeling like something is wrong with them when in reality, their nervous system is simply doing its best to protect them. You’re not broken—you’re wired for survival. And you can learn how to regulate, heal, and thrive.
I’m Kate Hagborg, LMHC, a therapist in Tacoma, WA and I’m here to help. Reach out today for a free 15-minute phone consultation.
Working with a therapist, especially one trained in brainspotting therapy, can be a powerful next step. Together, we can help your nervous system feel safer, your emotions more manageable, and your life more connected.
You’re ready for help—I’m a therapist in Tacoma, WA and I’m here for you
If you’re ready to begin your journey toward nervous system regulation, I’d love to connect. I offer a free 15-minute phone consultation so we can talk about what you’re looking for and see if we’re a good fit. Give me a call today—I’m here to help you feel more grounded, resilient, and whole.
Ask a Therapist in Tacoma: What Are Signs of a Dysregulated Nervous System?
Feeling overwhelmed, anxious, or just “off” without knowing why? You might be experiencing signs of a dysregulated nervous system. In this blog, a therapist in Tacoma breaks down the physical and emotional symptoms—like chronic fatigue, mood swings, hypervigilance, and freeze responses—and explains how they’re often connected to unresolved stress or trauma. You’ll also learn how Brainspotting therapy, a powerful somatic-based approach, can help you access and heal the deeper parts of the brain where dysregulation lives. Whether you’re dealing with burnout, anxiety, or just want to feel more grounded, this post offers real insight and practical steps to start feeling better. If you’re in Tacoma and looking for support, this guide is a compassionate, informative starting point—and it might just be the first step toward real, lasting change. Click to learn how Brainspotting therapy can help you feel more like yourself again.
Hey Tacoma—What Is a Dysregulated Nervous System, Anyway?
If you've ever felt overwhelmed for "no reason" or stuck in a cycle of anxiety and fatigue, you might be dealing with a dysregulated nervous system. As a therapist in Tacoma, I often explain this in simple terms: your nervous system is like your body's alarm and relaxation system. When it’s working well, it knows when to activate and when to calm down. But if it’s dysregulated, it can get stuck in overdrive or shutdown mode. That means your body and brain might respond to everyday stress as if it were a full-blown crisis. Therapies like Brainspotting can help identify where these stress responses are held in the body, gently supporting the nervous system in returning to balance.
Why Your Body Feels “Off” and You Can’t Explain It
One of the first clues that your nervous system might be dysregulated is a persistent sense of something being "off" in your body. Maybe you're exhausted even after a full night's sleep, or your muscles are constantly tense. Some folks feel a tight chest, shallow breathing, or frequent stomachaches. These are all signs that your body is trying to communicate something. As a therapist in Tacoma, I always encourage clients to trust what their body is telling them—it often knows before our minds catch up. Brainspotting works with that body awareness, allowing us to explore what’s stored in the deeper parts of the brain, beyond words.
Emotional Rollercoaster? Your Nervous System Might Be Involved
The mood swings of a dysregulated nervous system can feel like a rollar coaster—not the good kind. Finding a therapist in Tacoma can help.
Ever feel like you're swinging from calm to anxious to irritable in a matter of minutes? Emotional volatility is another hallmark of nervous system dysregulation. It doesn’t mean you're "too sensitive" or "overreacting"—your system is simply trying to protect you, even if there isn’t a clear and present danger. I often help clients in my Tacoma therapy office learn to notice these shifts without judgment, so they can start to understand what's going on underneath. Brainspotting can be especially helpful here because it targets the root of these emotional patterns—not just the symptoms.
Freeze, Fawn, Fight, or Flight—Which One Shows Up for You?
When we talk about trauma and nervous system responses, the four Fs—fight, flight, freeze, and fawn—often come up. Fight might look like snapping at someone unexpectedly. Flight might look like overworking or always being busy. Freeze can be zoning out or feeling paralyzed. Fawn might be people-pleasing to avoid conflict. These are all nervous system strategies designed to keep us safe. In therapy, we look at which patterns are showing up and why, so we can create space for new, healthier responses. Brainspotting helps by processing these responses at the source, unlocking stuck survival energy that keeps us cycling through the same reactions.
Therapist in Tacoma Explains: How Stress Hijacks Your Nervous System
When stress is chronic, it doesn’t just affect your mood—it impacts your entire nervous system. Think of it like your internal dashboard: too much pressure and the warning lights start flashing. Hormones like cortisol and adrenaline flood your system, and your brain has a harder time shifting into rest mode. In my work as a therapist in Tacoma, I see this often in folks who are juggling work, family, and life demands without a moment to reset. That constant "on" feeling can be draining. Brainspotting allows us to process the stress that’s built up over time, so your system can finally take its foot off the gas pedal.
When Coffee Feels Like a Panic Attack: Clues You Might Miss
If your nervous system is dysregulated, even small things can tip the scale. Some of my Tacoma clients report that caffeine suddenly makes them jittery or anxious, or that loud sounds feel unbearable. This kind of sensory sensitivity is a red flag. It means your system is already on edge, and even minor stimuli can feel overwhelming. You’re not crazy—you’re just maxed out. Recognizing this can be the first step toward healing. Brainspotting offers a gentle, non-verbal path to help your nervous system down-regulate, even when traditional talk therapy hasn’t helped.
Signs of a dysregulated nervous system can look like anxiety or depression—or both. Finding a therapist in Tacoma can help you address these symptoms.
Are You Always “On” or Totally Numb? That’s a Red Flag
Hypervigilance and emotional numbness might seem like opposites, but they both point to the same issue: nervous system dysregulation. If you're constantly scanning for danger, even in safe environments, your system might be stuck in a fight-or-flight state. On the other hand, if you feel emotionally flat or disconnected, you might be in freeze mode. As a therapist in Tacoma, I help people recognize these extremes and find ways to come back to center. Brainspotting can support this process by allowing your brain to process overwhelming or frozen experiences at a pace that feels safe.
Your Gut, Sleep, and Skin Are Talking—Are You Listening?
Your nervous system doesn't just live in your head—it's connected to your whole body. That means gut issues, skin flare-ups, and sleep disturbances can all be signs of dysregulation. If you’re waking up at 3 AM every night or dealing with chronic digestive issues, your nervous system might be trying to get your attention. Tacoma clients are often surprised to learn that addressing emotional health can improve physical symptoms too. Brainspotting helps us access those deeper layers of stored stress and trauma that are often behind persistent physical symptoms.
How a Therapist in Tacoma Can Help You Re-Regulate
Therapy can be a powerful tool for regulating your nervous system. In my Tacoma practice, I use approaches like Brainspotting, mindfulness, and somatic techniques to help clients reconnect with their bodies and emotions. It's not about "fixing" you—it's about helping your system feel safe enough to shift. Brainspotting in particular can be transformative because it works directly with the brain and body to release trauma and emotional blocks, often without needing to rehash painful stories. Over time, clients start to notice more calm, better sleep, improved relationships, and a greater sense of resilience.
Small Steps You Can Take Today to Soothe Your Nervous System
You don’t have to wait for a therapy session to start regulating your nervous system. Try placing your hand on your chest and taking slow, deep breaths. Go outside and feel your feet on the ground. Listen to calming music or splash cold water on your face. These might seem small, but they send powerful signals of safety to your brain. And when you're ready to go deeper, therapy—and especially Brainspotting—can offer lasting support. If you're in Tacoma and wondering whether Brainspotting therapy might be right for you, I invite you to reach out. Let’s talk about what you’re experiencing and explore how healing can begin.
Interested in Brainspotting therapy in Tacoma?
If any of this sounds familiar, you’re not alone—and you don’t have to figure it out by yourself. I specialize in helping people heal from nervous system dysregulation using Brainspotting and other approaches. Reach out today to schedule a free 15-minute consultation and explore whether Brainspotting might be the right fit for you.
The top 10 Truths about counselling, therapy, psychotherapy, and coaching in Tacoma, WA
This is Kate Hagborg, LMHC with Destiny City Counseling, and I’m your friendly neighborhood therapist in Tacoma, WA. Here are 10 truths about counseling that therapists like me wish you knew! What’s standing in the way of you changing your life? Call today for a free 15-minute phone consultation and start getting the support you need to feel better.
Therapy can be life-changing, but many people have misconceptions about what to expect. As a therapist in Tacoma, WA, I want to share 10 essential truths that can help you get the most out of your counseling experience.
1. Therapy Is for Everyone, Not Just Those in Crisis
You don’t need to be in a crisis to benefit from therapy. Many people seek counseling for self-growth, relationship challenges, career decisions, and personal development. Therapy is a proactive way to improve your mental and emotional well-being. Therapy can be like working out with a personal trainer—it’s a way to invest in your growth and get exponential results.
2. Healing Takes Time, But Small Steps Lead to Big Changes
Therapy isn’t a quick fix, but that doesn’t mean you won’t see results. Even small shifts in thinking and behavior can create lasting positive changes over time. Committing to the process is key. I encourage clients to give it 4-6 sessions. In that period of time, you probably won’t have met all of your goals, but you should feel noticeable changes. If not, talk to your therapist and go over your goals (also known as your treatment plan) with them again so you can be sure that you are getting everything you need from this process. With consistent effort over time, you’ll be amazed at the changes you can make in your mood, behaviors, relationships, and more.
3. Your Therapist Won’t Judge You—This Is a Safe Space
Many people hesitate to share their deepest thoughts and feelings, fearing judgment. But therapy is a judgment-free zone. A skilled therapist in Tacoma, WA creates a safe space where you can be your authentic self without fear. Our goal is to give you an experience of a relationship where you can explore your authentic self and feel totally safe, supported, and not judged. This helps you grow in compassion for yourself and make changes in your relationships with other people.
4. Therapy Isn’t Just About Talking—It’s About Transformation
Therapy isn’t just venting; it’s about learning tools to change your patterns, behaviors, and mindset. Techniques like brainspotting therapy go beyond words to help clients process trauma, anxiety, and emotional blocks on a deeper level. Brainspotting helps clients to change on the neurobiological level by working with both the brain and the body to get deeper and more lasting results.
5. You Don’t Have to Know Exactly What’s Wrong to Start Therapy
Many people think they need a specific reason to begin therapy, but that’s not true. If something feels off, you’re feeling stuck, or you just want extra support, therapy can help you gain clarity and direction. In the first couple of sessions, I work with clients to understand the context of their story, what they want for their future, and then to set goals for our time together. These goals will help us be specific about the changes you want to experience in your life, and a way for us to measure the effectiveness of our work together. If you’re not sure what you want to change, we can find that together.
6. Therapy Can Be Affordable—Even Without Insurance
Many therapists do not accept insurance, but that doesn’t mean therapy is out of reach. Here’s how you can afford therapy without in-network insurance:
Use Out-of-Network Benefits: Many insurance plans reimburse for therapy with an out-of-network provider.
Ask for a Superbill: A superbill is an invoice your therapist provides so you can submit it for potential reimbursement.
Use an HSA or FSA: Health Savings Accounts (HSA) and Flexible Spending Accounts (FSA) can often be used to cover therapy costs.
If you’re unsure about your insurance coverage, call your provider and ask about out-of-network mental health benefits.
7. You Don’t Have to Share Everything at Once—Go at Your Own Pace
It’s okay to take your time in therapy. You don’t have to dive into painful memories right away. A good therapist will respect your pace and help you feel comfortable before exploring deeper topics. As trust and rapport develop, we can get into areas that require more gentleness and support to process. Creating a treatment plan at the beginning of therapy allows us to determine our goals and priorities of what we want to work on now, and what we want to build up to later.
8. Your Therapist Won’t “Fix” You—Because You’re Not Broken
Therapy isn’t about fixing you—it’s about helping you understand yourself, heal, and grow. You already have strength and resilience; therapy just helps you tap into it. This is one reason that I love brainspotting therapy—it helps clients connect to their inner resiliency and resources. In brainspotting, when we lean in and honor the wisdom of your body expressed as emotions, somatic experiences, thoughts, memories, and intuition, brainspotting allows your body to naturally “unwind the knots” and get to a place of peace, acceptance, and growth.
9. Finding the Right Therapist Is Important—It’s Okay to Switch
Not every therapist will be the right fit for you, and that’s okay. If you don’t feel comfortable or understood, don’t be afraid to try a different therapist in Tacoma, WA who aligns better with your needs. If you’re working with a therapist and aren’t feeling aligned with the methods, seeing positive results, or feeling safe and understood, let them know. It can be awkward to broach these conversations, but your therapist is a professional and they will understand. A good therapist will welcome the feedback graciously and help adjust the approach to be the right fit for you. If that still isn’t working, you can talk to your therapist about the need to find a better fit, and they can even help you with referrals to find the right match. They want the best for you and this is absolutely an ok thing to do. As a professional, they should support you and celebrate your self-advocacy.
10. Therapy Works Best When You’re Open and Committed
The more you engage with the therapy process—both in and outside of sessions—the more benefits you’ll see. Therapy is a partnership, and your willingness to reflect, experiment with new coping skills, and practice self-awareness makes all the difference.
Your therapist can suggest ways you can practice what was discussed in your session throughout the week. They may also be able to suggest books, podcasts, or resources to support the work you are doing. If you like the idea of learning more between sessions, great!
If you are already busy and it’s overwhelming to think about adding anything in between sessions, don’t worry about it! This process is all about meeting you where you are in life. You and your therapist can maximize your sessions to get you to your goals without feeling like you have to complete homework assignments between sessions to be successful. The key is discussing what kind of support you want and making a plan with your therapist in line with that.
Ready to Start Therapy in Tacoma, WA?
If you’re thinking about therapy, don’t let doubts hold you back. Whether you’re interested in traditional counseling or specialized approaches like brainspotting therapy, finding the right therapist in Tacoma, WA can help you take the next step toward healing and growth.
I love working with women in Tacoma, WA to help them overcome people-pleasing and codependency, heal burnout, calm anxiety, and find peace again. Contact me today to schedule a free 15-minute phone consultation to see if we’d be a good fit to help you reach your goals.
The Top 8 Myths about counseling, coaching, psychotherapy, and therapy in Tacoma, WA
Are you on the fence about therapy? I’m Kate Hagborg, LMHC, and I’m a therapist in Tacoma, WA—here to help! In this article, I debunk 8 of the top myths that keep people stuck instead of accessing the mental health care that could help them feel better sooner.
Are you considering finding a therapist in Tacoma? But maybe you have some questions first?
Hi, I’m Kate Hagborg, LMHC, your friendly Tacoma therapist, and I’m here to help!
Counseling is an incredible tool for personal growth, healing, and self-discovery. Unfortunately, many people avoid therapy due to common misconceptions. Today, let’s clear up some of these myths so you can make informed decisions about your mental health.
1. Counseling Is Only for People With Serious Mental Health Issues
Many people believe that therapy is only for those struggling with severe mental health conditions like depression or anxiety disorders. You may be wondering, “Do my problems really compare to other people’s?” “Will a therapist just think I’m making a big deal over nothing"?”
In reality, people seek therapy for all kinds of reasons—stress, anxiety, relationship challenges, career transitions, or even self-improvement. Therapy is for everyone. A good therapist will never judge you for taking a brave help to make yourself better. And they won’t compare you to anyone either. Counseling can be an excellent way to get to know yourself better, improve your relationships, practice self-care, and more.
2. A Therapist in Tacoma, WA Will Just Listen and Not Offer Solutions
Some people think that therapy is just talking without any real advice or guidance. However, therapists use evidence-based techniques to help clients develop coping strategies, reframe negative thinking, and create actionable plans to improve their lives. Sometimes we may use talk therapy in sessions, and sometimes your therapist may introduce other tools to help you get to the root of your issue and experience positive changes.
As a therapist in Tacoma, one evidence-based technique I like to use that gets rapid, lasting, and deep results is something called brainspotting therapy.
What is Brainspotting Therapy?
Brainspotting is an innovative approach that goes beyond traditional talk therapy by working with both the mind and the body. This method helps clients access and process deeply stored trauma by using eye positions to activate the brain’s natural healing abilities. Brainspotting can be especially effective for people who feel stuck in talk therapy or struggle with anxiety, PTSD, and emotional blocks. But it’s effective at helping people break through to new levels of performance, work through relationship issues, feel more grounded, and increase their sense of peace in their daily lives.
To read more about brainspotting therapy in Tacoma, WA, check out these articles: Cultivating Self-Compassion Through Brainpsotting and How to Prepare for a Brainspotting Session.
3. If I’m Strong, I Shouldn’t Need Therapy
Thankfully, this myth is fading out more and more considering al the work recent generations have done in destigmatizing therapy and prioritizing taking care of one’s mental health. However, some people still believe that seeking therapy means they are weak.
In truth, asking for help takes immense strength. Even the “strongest people”—professional athletes, CEOs, and first responders, for instance—seek therapy to maintain their mental well-being. A therapist in Tacoma, WA can provide valuable support for anyone. Many highly successful individuals, including entrepreneurs, artists, and public figures, use therapy to maintain emotional balance and clarity. Therapy isn’t about weakness—it’s about self-improvement and growth.
4. Therapy Takes Years to See Results
You’d be surprised how much progress you can make in just a few short sessions. Short-term, goal-focused therapy can be highly effective for overcoming stress, anxiety, and relationship challenges.
In general, I tell clients they should experience some degree of positive change in their life within 4 sessions. While some issues require long-term therapy, these changes are a process and there are some benefits you can begin reaping early on in the journey.
It’s good to hold this in tension with knowing that healing is a process. Some things we come to therapy to address were years or decades in the making, and it’s understandable that thorough healing may also take time. But you shouldn’t have to wait forever to see some results.
5. Talking About My Problems Will Make Them Worse
Some people avoid therapy because they fear talking about their struggles will intensify their emotions. You may have heard of the term “toxic positivity.” This is when someone is probably well-meaning, and tries to “focus on the bright side” so much so that they end up suppressing, denying, or invalidating difficult feelings. Research shows that suppressing feelings often leads to greater distress. Just because you are acknowledging what is hard or painful doesn’t mean that you’ll end up stuck there. A skilled therapist helps clients process emotions in a healthy way, making them feel lighter and more in control.
6. A Therapist Will Judge Me
The fear of being judged keeps many people from seeking help. However, therapists are trained to provide a non-judgmental and safe space where clients can express themselves openly and honestly. My biggest goal in working with people is to create a safe and comfortable environment where you can explore your thoughts, feelings, and experiences in a shame-free space. Feeling empathy and compassion from someone like a therapist can pave the way for us to experience more self-compassion, which is another helpful outcome from therapy.
7. Counseling Is Too Expensive
Many people worry about the cost of therapy, especially if a therapist does not accept insurance. However, there are ways to make therapy more affordable:
Out-of-Network Benefits: Many insurance plans offer out-of-network reimbursement, which means you can see a therapist who doesn’t take insurance and still get partial reimbursement.
Superbills: I and many out-of-network therapists in Tacoma, WA provide a superbill (a detailed invoice for your insurance company), which you can submit for potential reimbursement.
Health Savings Accounts (HSA) or Flexible Spending Accounts (FSA): These accounts allow you to use pre-tax dollars for therapy sessions.
To find out about your insurance reimbursement for out-of-network mental health therapy, call the 1-800 number on the back of your insurance card. Ask them if you have coverage for out-of-network mental health and what it is. Ask if you have to meet a deductible first. And ask if they cover telehealth and in-person therapy equally.
8. If I Start Therapy, I’ll Have to Go Forever
There are a lot of better hobbies than going to counseling! Therapy isn’t a lifetime commitment. Many people benefit from short-term therapy, while others choose to continue for ongoing support. The duration of therapy depends entirely on your personal needs and goals. For me, within the first two sessions, my clients and I develop a treatment plan, which is like a roadmap to your goals. We determine what your goals are and how your life will look when you meet those goals. That way we can assess your progress along the way. From the beginning, we will talk about what it would look like for you to be ready to eventually graduate therapy, and work toward you seeing those positive changes together.
Find a Therapist in Tacoma, WA Who Fits Your Needs
If you’re considering finding a therapist in Tacoma, WA, don’t let these myths hold you back. Whether you’re interested in traditional counseling or specialized approaches like brainspotting therapy, finding the right therapist in Tacoma, WA can help you navigate life’s challenges with clarity and confidence. Ready to take the next step? Contact me today to schedule a consultation.
What to expect from counseling, mental health, psychotherapy, and therapy in Tacoma, WA
Finding a therapist in Tacoma, WA can be a daunting and overwhelming process, especially when you aren’t sure what to expect in therapy. Let me break down how therapy works and give you an idea of what to expect in your consultation call, your first therapy session, and in your on-going work with a therapist in Tacoma, WA.
So you’re looking for a therapist in Tacoma, WA.
You’ve been meaning to get around to finding a therapist for awhile now. You know therapy can help you, but it’s overwhelming to figure out who to work with. And you’re just a little bit nervous about going to therapy. Maybe you’ve never done it before and you don’t know what to expect. Maybe you’re thinking. “I don’t even know what I’m supposed to talk about!”
Or maybe you have tried therapy before, but the experience wasn’t everything that you were hoping for. You and your therapist didn’t connect very well, or the sessions just felt like chatting and rehashing your week over and over… Or maybe it was sort of helpful, but you still feel like you haven’t gotten to the root of your issues the way you wanted.
What to expect from starting therapy in Tacoma, WA.
I’m kate, a licensed therapist in Tacoma, WA, and I’m here to help.
I know finding a therapist can be a daunting and overwhelming process, especially when you aren’t sure what to expect in therapy. Let me break down how therapy works and give you an idea of what to expect in your consultation call, your first therapy session, and in your on-going work with a therapist in Tacoma, WA.
what to expect in a consultation call with a therapist in Tacoma, WA.
Most therapists offer a free 15-min consultation call in order to have a chance for them to hear more about what you’re looking for in counseling, answer any questions you might have, and together see if you would be a good fit to work together. Here’s how these calls usually work. First, you find some potential options for therapists you might like to work with. I’ve outlined ideas about how to do that here in this blog.
Then you reach out to the therapist either by picking up the phone and giving them a call, or filling out the contact form on their website. The therapist will get back to you and schedule a time to have the consultation call. These are usually free and often last about 15 minutes.
When the therapist calls you, they will often ask you to share a little bit about what you are hoping to work on in therapy. This is a chance to tell them a little about the symptoms you are experiencing, the challenges you are facing, or how you want life to improve. This can be hard to put into words sometimes. Maybe you are overwhelmed and don’t even know where to begin. Maybe talking about how you’re feeling or asking for help is hard, and it’s difficult to put it into words. Or maybe you’re doing your best to hold it all together, and as soon as you’re asked this question, you feel like you’re going to break down into tears. That is totally ok. We understand that this is a loaded question and it’s completely fine to get emotional. We also understand sometimes these things are hard to articulate. Just do your best to give the therapist a little snapshot. You don’t have to go into a lot of detail in this call. Just a few sentences about the challenges you are facing or the ways that you want life to be different is enough to give them an idea of what you want to address.
The therapist may ask you a couple of the following questions about how long you’ve been experiencing symptoms, if you are having thoughts of harming yourself or others, if you’ve tried therapy before, etc. This is just to get a better idea of the kind of help you are looking for and if they are the right person to help you.
Remember that the consultation call is a chance for you to also ask whatever questions you have. You are interviewing them, too! Things you might want to know:
Have you worked with someone who has had my issue before? Was it a successful outcome?
Do you have specialized training in working with my issue?
What type of therapy do you do and how does it work?
What should I expect in terms of how we work together to improve this issue?
For people with my issue, about how long should I expect to be in therapy for?
After you and the therapist discuss a little about the issues you want to address, you can both decide if you want to move forward to set up the first session, called the intake session. You want to assess if this person seems like they have the experience and expertise to help you. You also want to get a vibe of their personality. Do you feel comfortable talking to them? Do they sound like someone you can imagine building trust with? The most important factor in successful therapy is the relationship between the therapist and the client. So be choosy! I tell clients it’s sort of like dating. You can expect to have to go on several dates to find a good match. Similarly, I encourage clients to do several consultation calls with different therapists to get a sense of who makes you feel comfortable.
The therapist will also be assessing if it feels like a good fit on their end. What that means is that they want to be sure they have the experience and expertise to help you. Mental health is a broad field, and not every therapist will work with every issue. Many therapists specialize in certain issues or working with certain populations. This way they can focus their training on providing excellent care in a few areas. For instance, some therapists focus on working with disordered eating, while others focus on addiction, or working with couples.
For me, I focus on helping people decrease anxiety and depression, break codependent patterns in relationships, and stop people-pleasing and build self-esteem. I like to use brainspotting therapy as my method because it helps people get long-lasting and rapid results in a deeper way than talk therapy can provide.
So if it feels like a good fit on both ends, then you and the therapist can discuss things like scheduling, the fee for services, insurance, and other practical details. If you are a good match in terms of these details, then you can schedule the first appointment.
What to expect in the first therapy session with a therapist in Tacoma, WA
When you start therapy in Tacoma, WA, the first session is known as the intake session. It’s a chance for the therapist to get to know more of your story and get the big picture of what you are experiencing and what you hope will change as a result of therapy. Beforehand, you may be asked to fill out some forms. These will include the therapist’s policies, an informed consent document, a questionairre about your symptoms and experiences, and possibly some assessments to determine if you meet the criteria for anxiety, depression, or other mental disorders.
When looking for a therapist in Tacoma, finding someone you trust and feel comfortable with is important.
During the session, the therapist will ask questions about what you’ve been experiencing to go into a deeper dive of your symptoms and how they are impacting your functioning in different enviornments. They will ask about different areas of life including your mood, behaviors, health, relationships, work life, social life, and family of origin. They are trying to get to know you as a person and understand your context and different factors that are contributing to your challenges. They are also listening for your support network, your resources, strengths, and resiliencies.
In the intake, you will also cover your goals for therapy. What are your best hopes for how therapy will help improve your life? If this is successful, what will feel different about your mood, your behaviors, your relationships, etc? The more specific you can be in naming what you hope can change, the better you and your therapist can set realistic, tangible goals. These goals are like mile-markers on a road trip. They enable you and the therapist to check-in along the way to see actual progress. If you are not seeing progress, you and your therapist can adjust the course as you go to make the process more effective for you. Or if it isn’t a good fit, you or the therapist could request a referral to get you the right help so you can achieve the progress you’re looking for.
If you’re not sure what tangible change would look like for you—don’t worry! Your therapist can help you articulate these goals. Sometimes all we can think about at first is just getting out of pain, and that’s enough of a goal to start with. When you start feeling better, you may have an easier time thinking of the positive changes you want to see in your life. You and your therapist can always adjust your goals as you go along in therapy.
One of the most important things about the first session is that you feel comfortable with your therapist. Just like in the consultation call, you want to be asking yourself if this is someone you feel like you can trust. Feel free to ask questions you have about the process of therapy, the therapist’s training, or whatever else you’d like to know. At any point, after the intake or at any time in therapy, if you’re not sure this is the right fit, bring it up to your therapist so they can discuss it with you. They may be able to make the changes you need to make you more comfortable and the therapy more beneficial for you. And if not, they are a professional, and will not be offended if you want to change course and try another therapist. This sort of thing happens frequently, so don’t feel bad if that’s what you need to do.
What to expect in your on-going therapy with a therapist in Tacoma, WA
Now that you and your therapist have your goals, the work can begin. Different therapists work in different ways, using different therapies to help their clients achieve their goals. I like to blend a few things together to help clients make progress.
Finding a therapist in Tacoma can help you grow in self-compassion.
An approach of self-compassion. No matter who I work with, this is a theme of working with me. I like to help clients cultivate deeper self-compassion. We can often be our own harshest critics. In whatever work I’m doing, I aim to help clients experience more empathy and kindness towards themselves which greatly helps the healing process.
Strengths-based approach. In therapy, it’s important to not just focus on the problems, but also where your strengths are. These strengths are proven resources that we can utilize to help you overcome whatever challenges you are currently facing. I frequently ask my clients what is improving in their life and we take time to celebrate the wins along the way, which increases their confidence in their ability to overcome the current problems and keep making progress.
A trauma-informed approach. Trauma doesn’t just impact our emotions—it affects us deeply on a psychological and physical level, too. That’s why it’s often not enough to just talk about things and hope they get better. Trauma is an injury to the brain and nervous system, and it takes an approach that engages the brain and nervous system to help you heal at the deepest level. That’s why I like to use brainspotting to help clients to heal trauma, decrease depression and anxiety, and change negative core beliefs and deeply rooted patterns. Brainspotting is a neuroscience-based approach that’s very effective for a wide variety of issues. Once we have the treatment plan of your goals, this is one of the tools we will use to help you start feeling better fast.
Along the way, you and your therapist should check-in regularly on your progress. If you are not noticing tangible differences after 3-6 sessions, then a course correction in the methods of therapy may be necessary to help you get more out of therapy.
The length of time in therapy depends on your goals. For some people it’s a few weeks, for others it is years. For most, it’s somewhere in between. I let clients know they should start feeling a positive change within 4-6 sessions, and significant progress after 4-6 months of weekly sessions.
In the beginning of therapy I like to ask my clients how they will know they are ready to graduate. Therapy in many cases does not have to be forever! We want to get you feeling better as quickly as we can and help you feel empowered with a new set of tools to navigate challenges. So progress should be part of this process. We will keep checking in until your goals are reached and you are ready to graduate.
so you’re ready to start therapy in Tacoma, WA
I hope this has helped ease some of your fears about starting the process of therapy and finding a therapist in Tacoma, WA.
I offer online therapy in Washington state. My specialties include helping people break out of people-pleasing, start healing their burnout, develop skills to overcome anxiety, and grow in self-compassion and appreciation for the awesome person they are. If you’d like to see if we are good fit to work together, reach out for a free 15-minute phone consultation.